Lower extremity arterial disease (LEAD)
Healthcare
About This Information:
This English version is a translation of content originally created based on medical information used in Japan. Accordingly, the data and treatment approaches presented reflect the situation in Japan and may differ from those in other countries or regions.
Supervised by: Dr. Shigeru Nakamura (Vice President and Director, Cardiovascular Center, Kyoto Katsura Hospital)
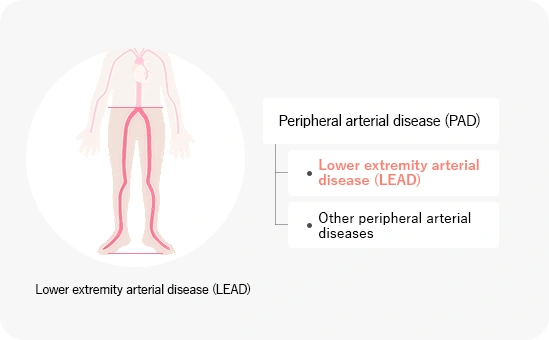
The blood flows from the heart through the large arteries (aortae) and to the brain, organs, hands, and legs. The blood vessels that extend down the arms and legs are called peripheral arteries.
Peripheral arterial disease (PAD) is a disease involving a narrowing of the arteries that travel to the arms and legs. Arteriosclerosis is more likely to occur in the legs than in the arms; when only the blood vessels that travel from the abdominal aorta to both legs are involved, the disease is called lower extremity arterial disease (LEAD).
Symptoms of lower extremity arterial disease (LEAD)
Lower extremity arterial disease is classified into four stages based on symptoms.
Fontaine classification
This is the evaluation criteria proposed by a German doctor, Dr. R. Fontaine, in 1954.
|
Classification |
Symptoms |
Main characteristics |
|---|---|---|
|
Stage I |
Asymptomatic or symptoms that may not be apparent. |
Patients are asymptomatic, or their toes feel cold and numb. These symptoms may occur regularly and may not be considered pathological. |
|
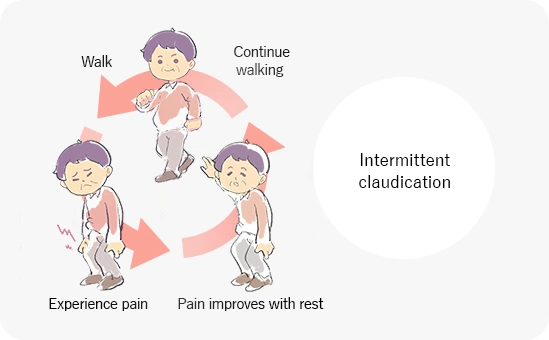
Stage II |
Intermittent claudication |
Patients usually experience pain and/or numbness in their legs after walking a certain distance. The symptoms disappear with rest. The leg muscles need a large amount of blood when walking, and poor blood circulation deprives them of oxygen, resulting in pain. Symptoms disappear at rest because the amount of blood required decreases. |
|
Stage III |
Pain at rest |
Extremely poor blood flow in the legs causes leg pain even when at rest. The pain interferes with sleep at night. |
|
Stage IV |
Ischemic ulcers or gangrene |
When the blood vessels are nearly completely blocked, an ulcer (wound) develops on the leg or the leg tissues necrotize (die). If infected, bacteria may spread throughout the body, causing a risk of death. A leg amputation may be necessary. |
Causes and risk factors of lower extremity arterial disease
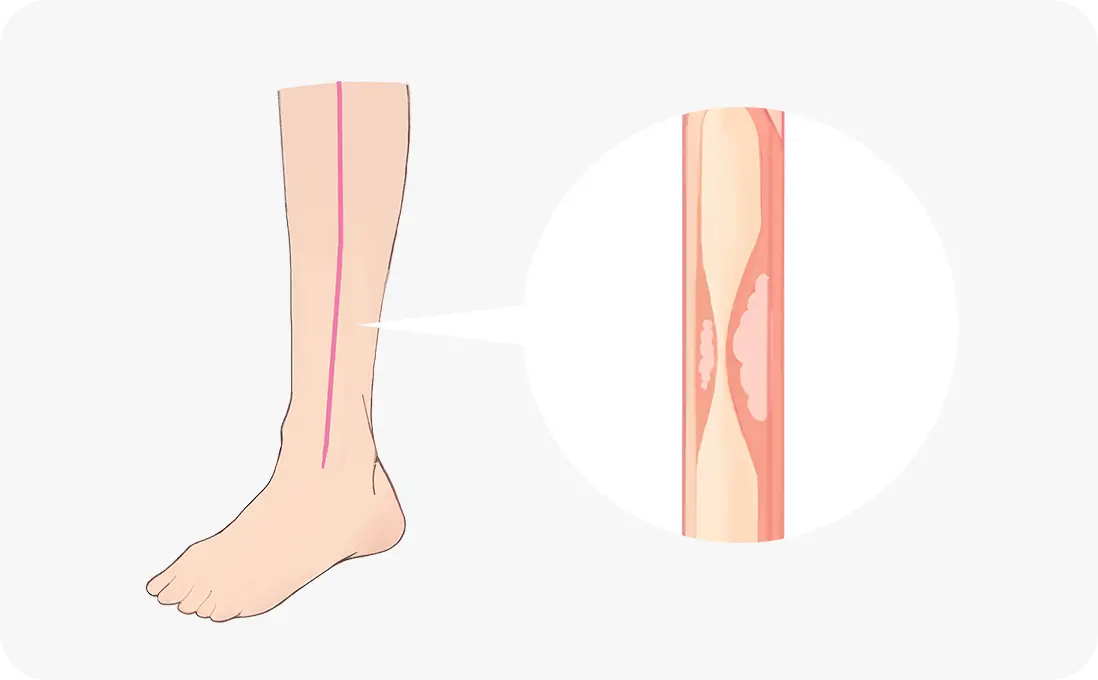
Arteriosclerosis causes lower extremity arterial disease.
When cholesterol and lipids build up on the inner lining of a blood vessel, the blood vessel hardens and becomes inflexible. As a result, it also narrows. People who smoke or have an underlying condition such as diabetes, hypertension, or dyslipidemia (high cholesterol) are significantly more likely to develop arteriosclerosis. Patients with diabetes are 3–4 times more likely to be affected by peripheral arterial disease.
In addition to arteriosclerosis in the arteries of the legs, people with lower extremity arterial disease are more likely to have concurrent arteriosclerosis (an incidence of 50%) in the blood vessels of the heart and the brain, which is associated with an increased risk of myocardial infarction and stroke. If lower extremity arterial disease is found, arteriosclerosis may also be present throughout the blood vessels of the body. Consequently, the whole body should be checked for arteriosclerosis.
Arteriosclerosis in patients on dialysis
When renal function is lost due to renal failure, life is sustained with dialysis treatment. However, the balance between calcium and phosphorus metabolism can easily be disrupted, and arteriosclerosis is more likely to progress throughout the body. For this reason, periodic testing should be performed in patients on dialysis for early detection and treatment of arteriosclerotic diseases, which can help maintain the quality of life (QOL) of these patients.
Acute limb ischemia (ALI)
Lower extremity arterial disease occurs when blood flow is gradually reduced due to arteriosclerosis of the peripheral vessels. If the blood flow is abruptly interrupted in the lower limbs, the disease is called acute limb ischemia. Unlike lower extremity arterial disease, acute limb ischemia requires emergency treatment.
The two main causes of acute limb ischemia are embolism and thrombosis.
Causes of acute limb ischemia
Embolism
Embolism is a condition in which a peripheral artery is suddenly blocked by a blood clot (thrombus) that formed in the atria; this primarily occurs in patients with arrhythmia (atrial fibrillation). If the clot travels to the brain, it causes an ischemic stroke.
Thrombosis
Thrombosis occurs when blood clots form in the already narrowed leg artery, eventually blocking it. A thrombus may also form in a tear in the wall of an artery (arterial dissection) or in an artificial blood vessel (graft) used for bypass surgery.
Symptoms of acute limb ischemia
Acute limb ischemia is a condition that requires emergency treatment. It commonly presents with five symptoms. If you experience any of these symptoms, visit a medical institution immediately.
The five symptoms of acute limb ischemia are named the 5 Ps because the English words all begin with the letter P.
|
Pain (pain in the affected limb) |
A sudden intense pain. Tingling pain remains even at rest. |
|---|---|
|
Pallor (pale skin) |
The skin on the leg and toes turns pale. As the disease progresses, the skin turns purple or black. |
|
Pulselessness (absence of pulse) |
A pulse is not found in the ankle or back of the knee. |
|
Paresthesia (loss of sensation) |
The leg is numb and becomes less sensitive as the disease progresses. Cold temperatures or pain cannot be felt. |
|
Paralysis (motor paralysis) |
The leg and toes are paralyzed and cannot be moved without help. |