Treatment of angina and myocardial infarction
Healthcare
About This Information:
This English version is a translation of content originally created based on medical information used in Japan. Accordingly, the data and treatment approaches presented reflect the situation in Japan and may differ from those in other countries or regions.
Supervised by: Dr. Shigeru Nakamura (Vice President and Director, Cardiovascular Center, Kyoto Katsura Hospital)
Angina treatment includes drug therapy, heart catheterization, and coronary artery bypass surgery.
For myocardial infarction, restoring blood flow as soon as possible is critical; therefore, emergency catheterization is performed.
Drug therapy
Antiplatelet drugs are used to prevent blockages cause by blood clots, and vasodilators are used to improve blood flow.
The aim of drug therapy for ischemic heart disease is to improve oxygen supply to the heart, relieve symptoms, and prevent disease progression.
| Blood thinners |
Antiplatelet drugs |
Suppress platelet function, thereby preventing blood clot formation in blood vessels. |
|---|---|---|
| Drugs that reduce the heart’s workload |
Beta-blockers |
Slow the heart rate, reduce the heart’s workload, and reduce oxygen demand. |
| Drugs that dilate blood vessels |
Nitric acid drugs, nitrous acid drugs, and calcium-channel blockers |
Dilate the coronary arteries and increase blood supply. |
| Drugs that lower blood pressure |
ACE inhibitors and ARB |
Lower blood pressure and reduce the heart’s workload, thereby protecting heart function. |
| Drugs that lower cholesterol |
Statins |
Reduce blood cholesterol levels and slow the progression of ischemic heart disease. |
Treatment is chosen based on the severity of symptoms and myocardial ischemia. Consult with your doctor to determine the best treatment strategy.
Percutaneous Coronary Intervention (PCI)
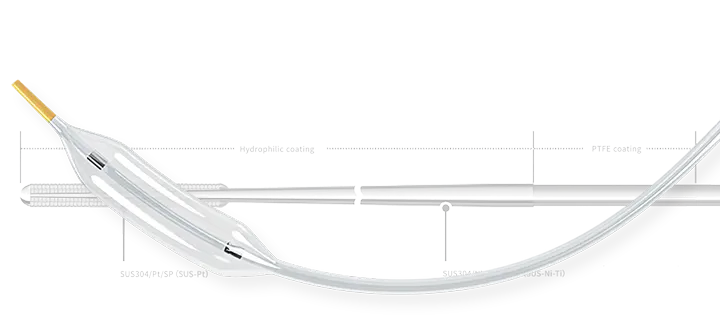
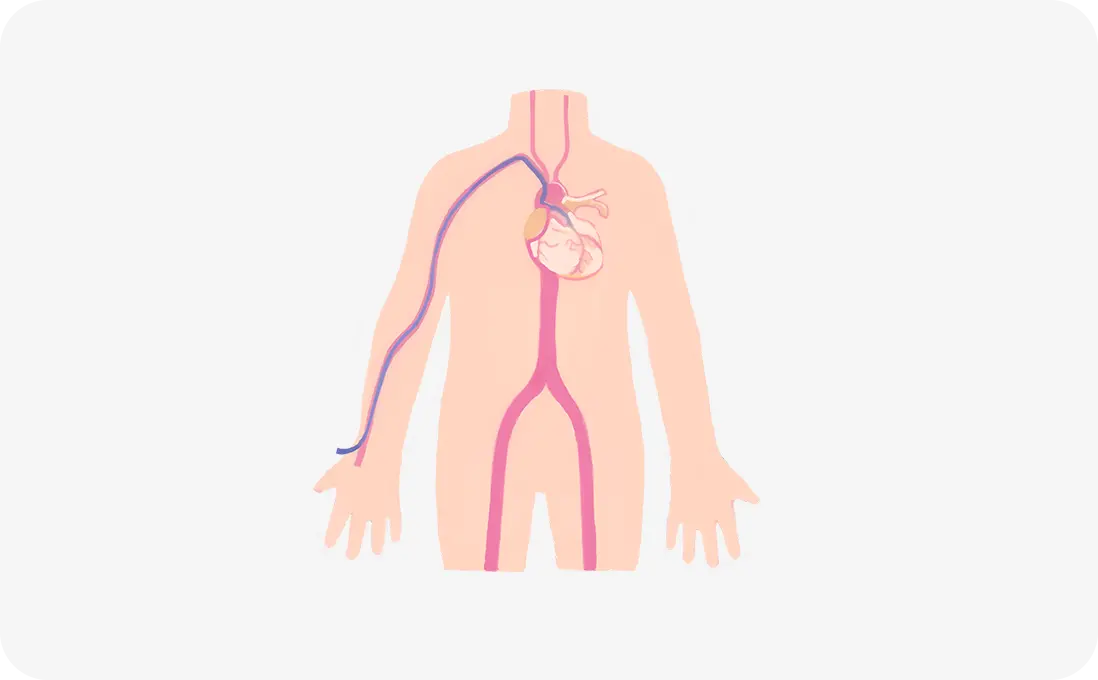
Coronary catheterization is a treatment in which a thin tube called a catheter is inserted into the coronary artery via the base of the wrist or foot to widen narrowed areas and improve blood flow.
The first non-surgical catheterization procedure was performed in Switzerland in 1978.
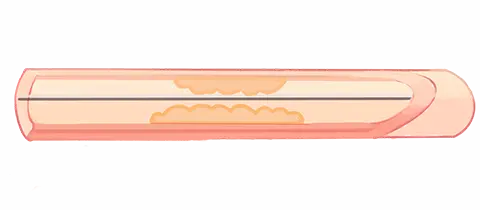
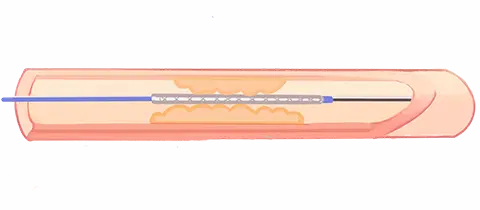
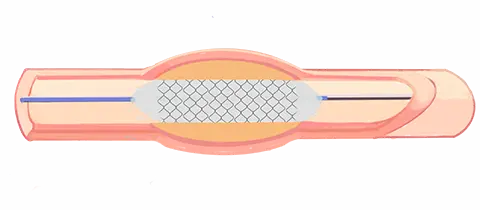
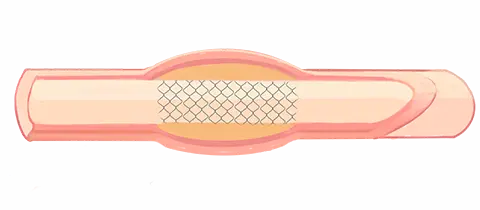
A thin guide wire, approximately 0.4 mm in diameter, is passed through a catheter into the coronary artery and through the narrowed area. Using this guide wire as a rail, a catheter with a balloon attached to the tip (balloon catheter) is threaded into the narrowed area. The balloon is then inflated to dilate the narrowed blood vessel from the inside. However, blood vessels are elastic and may recoil after dilation. To prevent this recoil, a metal mesh tube is placed in the blood vessel at the same time as the balloon to support the dilated vessel from the inside. This device is called a stent.
PCI stenting
|
|
|
|
|---|---|---|---|
|
1. Pass the guide wire through the narrowed area. |
2. Insert the balloon catheter and stent. |
3. Inflate the balloon and expand the stent. |
4. Deflate and remove the balloon while retaining the implanted stent. The surface of the stent is coated with a drug to prevent restenosis. |
Coronary Artery Bypass Grafting (CABG)
Coronary artery bypass is a surgical treatment in which a bypass blood vessel is connected below the narrowed area using an artery from the chest cavity or a vein from the leg; this bypass vessel improves blood flow to the restricted area.
Coronary artery bypass is a surgical procedure that creates a new path (bypass) for blood to flow beyond the narrowed or blocked coronary artery. This procedure was first performed in the United States in 1967. It was a groundbreaking innovation, enabling blood to perfuse the ischemic myocardium.
The heart is temporarily stopped, and a leg vein is connected to the coronary artery while a device called a heart-lung machine pumps blood through the body. In recent years, a procedure for connecting the graft vessel to the coronary artery without stopping the heart has also been widely employed.
The leg vein used for bypass has a lifespan of approximately 10–20 years. Therefore, they are currently used in combination with an artery from the chest cavity, which has favorable long-term patency outcomes.
In comparison with catheterization, bypass surgery is performed in patients with diabetes or for more complicated lesions. This surgery has been reported to provide a favorable prognosis.
CABG involves a large incision in the chest under general anesthesia. As a result, the hospital stay is longer than that after catheterization.